Service innovation.
Supporting patients to quit or reduce smoking
Despite Australia having one of the lowest smoking rates in the world, people experiencing homelessness are eight times more likely to smoke than the general population. Among patients seen by Homeless Healthcare (HHC), 79% currently smoke and 11% previously smoked. Given the enormous health consequences of smoking, barriers to accessing cessation support further entrenches health inequalities experienced by people who are homeless in Australia.
As tobacco dependence is often high in the homeless population, Nicotine Replacement Therapy (NRT) can play an important role in supporting quit attempts, but the NRT options available on the Australian Pharmaceutical Benefits Scheme (PBS) are limited. Since March 2020, Homeless Healthcare has been supported by the Cancer Council of WA to provide patients who smoke with no-cost access to NRT. This has significantly broadened the range of NRT products that can be prescribed, increased the duration of NRT support available, and removed the cost of NRT as a barrier to cessation.
The initial pilot to trial this NRT support was evaluated by the Home2Health team from the University of Notre Dame. During the 2 year evaluation, (April 2020- March 2022), 305 Homeless Healthcare patients were supported to quit or reduce their smoking with the assistance of NRT funded by the Cancer Council. This generous funding support has continued, and no-cost NRT is now also available to patients supported by HHC at the Medical Respite Centre.
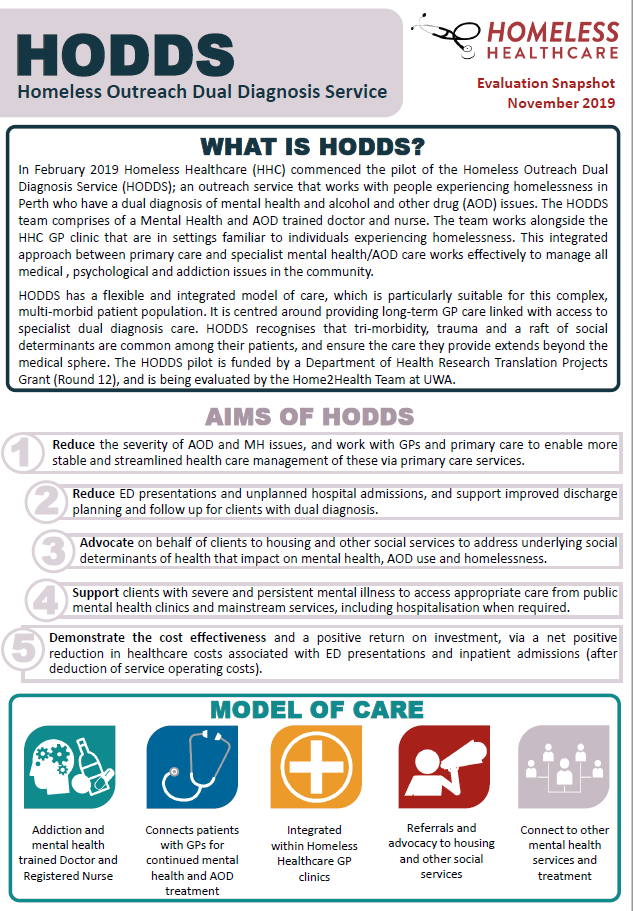
Homeless Outreach Dual Diagnosis Service (HODDS)
Homeless Healthcare ( commenced the pilot of the Homeless Outreach Dual Diagnosis Service ( an outreach service that works with people experiencing homelessness in Perth who have a dual diagnosis of mental health and alcohol and other drug ( issues The HODDS team comprises of a Mental Health and AOD trained doctor and nurse The team works alongside the HHC GP clinic that are in settings familiar to individuals experiencing homelessness.
HODDS has a flexible and integrated model of care, which is particularly suitable for this complex, multi morbid patient population It is centred around providing long term GP care linked with access to specialist dual diagnosis care HODDS recognises that tri morbidity, trauma and a raft of social determinants are common among their patients, and ensure the care they provide extends beyond the medical sphere.
If you’d like more information on HODDS, see below for the independent evaluation of the HODDS program, and HODDS article published in Parity Magazine.
‘Dual diagnosis in people who are homeless is often rooted in childhood trauma; alcohol and drugs are frequently used to regulate mood and emotions associated with trauma and the severe adversity of homelessness. Practical issues can also perpetuate AOD use – for example, women who use meth to keep awake on the streets at night when it is most dangerous.’
— Entwined mental health and AOD issues, Clinical Lead, RPH Homeless Team
Medical Respite and Recovery Centre
StayWitch’s is Homeless Healthcare’s recently opened post-hospital medical respite and recovery facility, which aims to provide a therapeutic respite environment for recently discharge patients who are experiencing homelessness. The centre provides a comfortable and medically supervised setting allowing for physical and psychological recovery, as well as creating opportunities for peer support, life-skills building whilst also connecting patients to additional social support services and long-term housing. This centre responds to a critical void in homelessness services, with homeless patients often facing a distinct lack of appropriate accommodation to go after hospital care. Many patients are ultimately discharged back onto the streets and the very conditions that placed them in hospital in the first place.
The centre provides an important stepping stone in a patients pathway to recovery and provides a ‘one-stop-shop’ for medical and social service support.
The below case study (written before HHC established StayWitch’s) highlights the huge need for such a facility in Perth.
Case Study: Unresolved Health Conditions and the Need for a Medical Recovery Centre in Perth
Background
Liam is a young male in his early twenties who has been cycling in and out of homelessness for at least four years. He has multiple co-morbidities including diabetes, depression, asthma, dental problems, mobility and learning difficulties. He has been on the waiting list for 50 Lives since June 2018 but needs a single bedroom unit and these are in scarce supply. His medical records indicate that he has been advised to use insulin four times a day and to store it in a fridge – an impossibility when living on the street.
Health Service utilisation and cost
Liam has presented to ED 33 times (26 at RPH) since 2016. He has also spent 31 nights as an inpatient with 90% of these being in the past year. His increasingly frequent hospital attendances relate particularly to his diabetes. In the last 11 months (March 2018 to February 2019), he has attended ED 15 times (10 at RPH) and been admitted for 19 nights, equating to a cost of $63,117.*
Liam has many complex mental and physical health concerns, however by the nature of ED, it is usually only the presenting and immediate issue that is addressed before discharge. In the past 15 presentations to ED, 13 of these have been recorded as diabetic related. This equates to $9,945 in preventable ED presentations for a condition that could be far better managed if he was housed and had a fridge for storing his insulin. Other health issues such as his asthma and schizophrenia could also be potentially stabilised with housing and GP support.
Benefits of a Medical Recovery Centre for this patient
Liam’s diabetes continues to worsen as reflected in the recurrent cycle of ED presentation and discharge. Given the medical uncertainty about his type of diabetes and his other health issues, if Perth had a Medical Recovery Centre he could be discharged to it for a period, enabling his diabetes to be further investigated and stabilised, and his mental health care reviewed.
Homeless Healthcare’s StayWitch’s facility